Allergic rhinitis
At a Glance










How It Affects You
Allergic rhinitis involves an inflammatory response primarily localized to the upper respiratory tract and face, occurring when the immune system overreacts to airborne particles. This reaction leads to swelling and irritation of the internal nasal membranes, causing congestion and mucus production, while also frequently affecting the conjunctiva of the eyes. Systemic effects, such as fatigue and irritability, often result from the physical discomfort and sleep disruption associated with these symptoms.
- Inflammation affects the nasal passages, sinuses, and throat.
- Ocular symptoms include itching, redness, and watering of the eyes.
- Sleep quality and cognitive function may be reduced due to persistent congestion.
Causes and Risk Factors
Underlying Causes and Mechanisms
Allergic rhinitis occurs when the body's immune system mistakenly identifies harmless airborne substances as dangerous intruders. Upon exposure to these substances, known as allergens, the immune system produces immunoglobulin E (IgE) antibodies. These antibodies attach to mast cells in the nasal passages and signal them to release chemicals such as histamine and leukotrienes. This chemical release causes the lining of the nose to become inflamed and swollen, leading to increased mucus production and the classic symptoms of allergies.
Triggers and Risk Factors
The specific triggers for allergic rhinitis vary depending on whether the condition is seasonal or perennial (year-round). Common triggers and risk factors include:
- Seasonal allergens: Pollen from trees, grasses, and weeds, which fluctuate depending on the time of year and geographic location.
- Perennial allergens: Indoor substances such as dust mites, pet dander (skin flakes), cockroach residue, and mold spores.
- Family history: Having a parent or sibling with allergies or asthma significantly increases the risk of developing the condition.
- Co-existing conditions: Individuals with eczema (atopic dermatitis) or asthma are more prone to developing allergic rhinitis.
Prevention Strategies
While it is not always possible to prevent the onset of the allergy itself, the primary method for preventing symptoms is avoidance of known triggers. Strategies to reduce exposure and prevent flare-ups include:
- Keeping windows closed during high pollen seasons and using air conditioning to filter indoor air.
- Washing bedding weekly in hot water to eliminate dust mites.
- Using high-efficiency particulate air (HEPA) filters in vacuum cleaners and air purifiers.
- Bathing pets regularly and keeping them out of bedrooms to minimize dander exposure.
- Monitoring local pollen counts and limiting outdoor activities when counts are high.
Diagnosis, Signs, and Symptoms
Signs and Symptoms
Symptoms of allergic rhinitis typically manifest immediately after exposure to an allergen. The most clinically meaningful signs involve the nose and eyes. Common symptoms include repetitive sneezing, a runny or stuffy nose, and intense itching of the nose, roof of the mouth, throat, or ears. Ocular symptoms, known as allergic conjunctivitis, frequently accompany nasal symptoms and include red, watery, and itchy eyes. In chronic cases, physical signs may appear, such as dark circles under the eyes (allergic shiners) and a horizontal crease across the nose caused by frequent upward rubbing.
Diagnostic Methods
Clinicians generally identify allergic rhinitis through a combination of medical history and physical examination. During the exam, a doctor may look for pale or bluish swollen nasal linings. To confirm the diagnosis and identify specific triggers, the following tests are often used:
- Skin prick test: Small amounts of suspected allergens are pricked into the skin of the arm or back; a raised bump indicates a positive allergic reaction.
- Specific IgE blood test: A blood sample is analyzed to measure the immune system's response to specific allergens, used when skin testing is not feasible.
Differential Diagnosis
It is important to distinguish allergic rhinitis from other conditions with similar symptoms. The common cold, caused by a virus, typically includes a fever and resolves within a week, whereas allergic rhinitis does not cause fever and persists as long as the allergen is present. Sinusitis involves facial pain and thick, colored discharge, unlike the clear, watery discharge typical of allergies. Non-allergic rhinitis mimics allergy symptoms but does not involve an immune reaction or identifiable allergens.
Treatment and Management
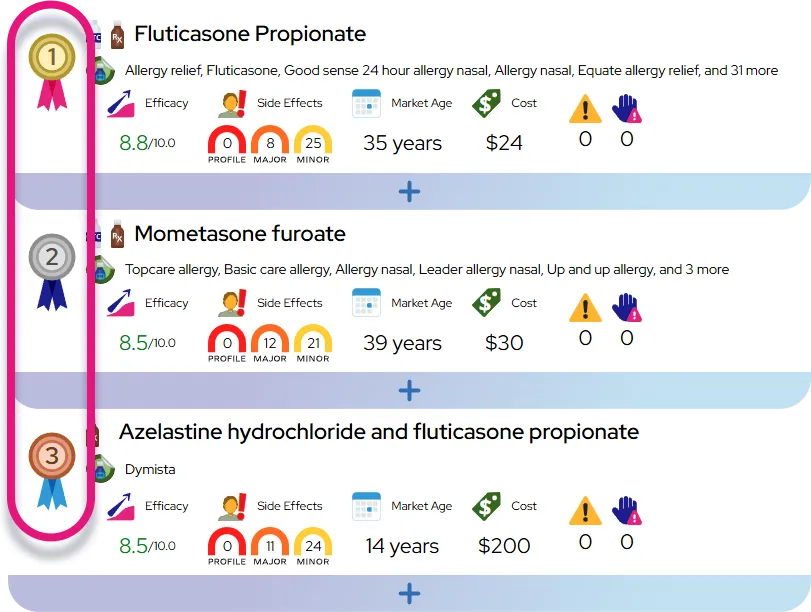
Medications
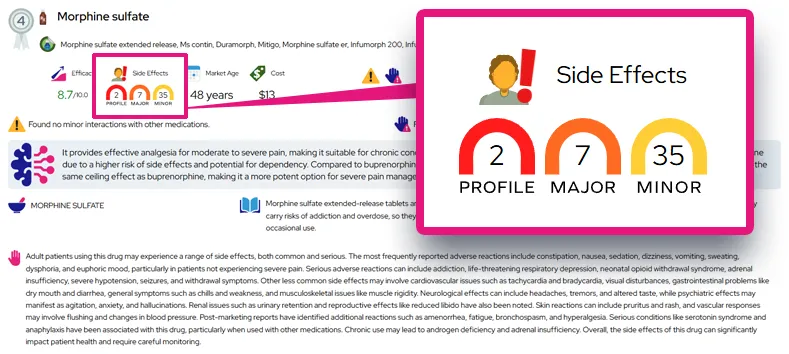
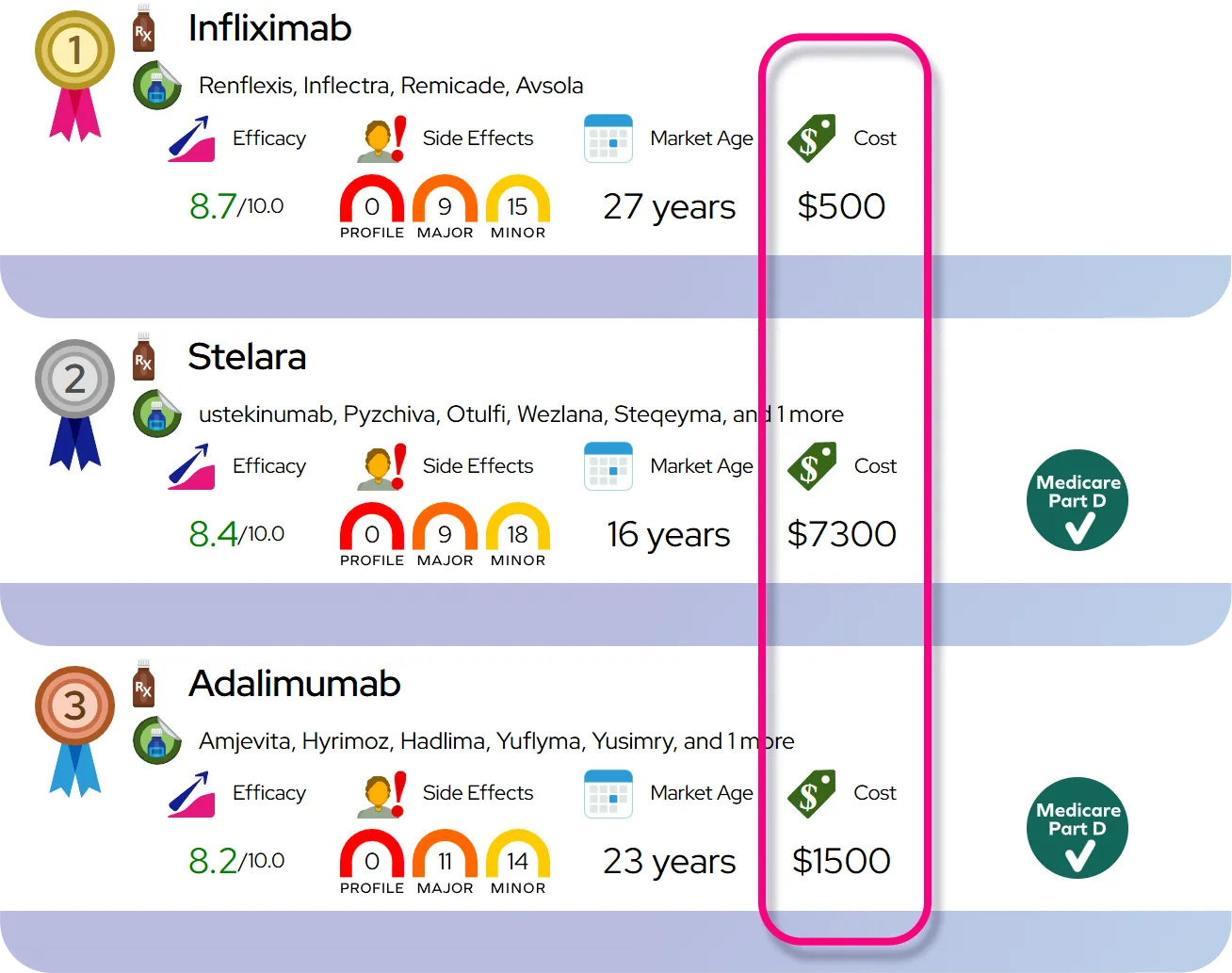
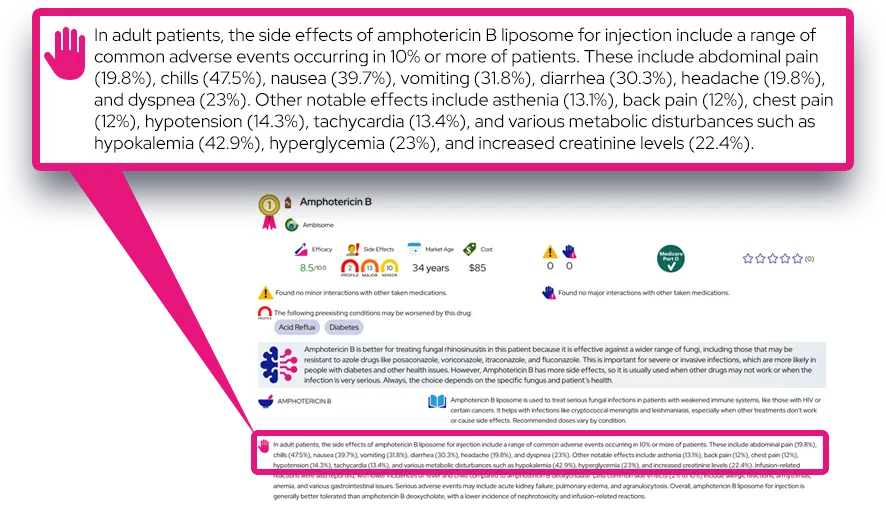
Pharmacological treatment focuses on reducing inflammation and blocking the immune response. Intranasal corticosteroids are often the most effective treatment for controlling chronic symptoms, reducing both congestion and inflammation. Antihistamines, available in oral pills, nasal sprays, or eye drops, help block histamine to relieve itching, sneezing, and runny nose. Decongestants can provide temporary relief for nasal stuffiness but are generally recommended only for short-term use due to potential side effects like rebound congestion.
Procedures and Therapies
For patients whose symptoms are not well-controlled by medications or who wish to reduce long-term medication use, allergen immunotherapy may be recommended. This involves exposing the body to gradually increasing amounts of the allergen to build up tolerance. This can be administered via subcutaneous injections (allergy shots) or sublingual tablets (under the tongue) and is the only treatment that can alter the natural course of the allergic disease.
Lifestyle and Self-Care
Management often begins with environmental control measures to minimize allergen exposure. Additionally, nasal saline irrigation using a squeeze bottle or neti pot can effectively rinse out mucus and allergens from the nasal passages. This simple home remedy helps clear the sinuses and soothe irritated membranes.
When to See a Doctor
Most cases of allergic rhinitis can be managed with over-the-counter remedies, but professional care is needed in certain situations. You should seek medical advice if:
- Symptoms are severe enough to disrupt sleep, work, or school despite home treatment.
- Over-the-counter medications cause troublesome side effects.
- Symptoms are accompanied by severe sinus pain, fever, or difficulty breathing.
- You suspect complications such as a sinus infection or worsening asthma.
Severity and Prognosis
Severity and Disease Course
Allergic rhinitis ranges from mild, intermittent nuisance symptoms to severe, persistent issues that significantly impair daily functioning. The condition is often classified based on duration (intermittent vs. persistent) and severity (mild vs. moderate-severe). While the condition is often lifelong, the severity of symptoms can wax and wane over time. Many children find their symptoms improve as they reach adulthood, though it is also possible for allergies to develop or return later in life. It is strictly a chronic condition of morbidity, meaning it affects quality of life but does not directly increase mortality risk.
Complications
Although allergic rhinitis is not fatal, uncontrolled inflammation can lead to several complications. It is a major risk factor for the development and worsening of asthma; poorly managed allergies often make asthma control more difficult. Other complications include acute or chronic sinusitis due to blocked nasal drainage and otitis media (middle ear infections), particularly in children. Chronic mouth breathing caused by nasal congestion can also lead to dental issues or facial structural changes in growing children.
Prognosis
The long-term prognosis is generally very good. With proper identification of triggers and adherence to treatment plans, most individuals can achieve near-complete symptom control. Modern treatments, including immunotherapy, offer the possibility of long-term remission for many patients. Early intervention can help prevent the progression of the disease and reduce the risk of associated complications like asthma.
Impact on Daily Life
Impact on Daily Activities
The symptoms of allergic rhinitis can be intrusive, affecting various aspects of daily life. Persistent congestion and sneezing often lead to poor sleep quality, which results in daytime fatigue, irritability, and difficulty concentrating. In school-aged children, this can manifest as behavioral problems or a decline in academic performance. For adults, untreated allergies are associated with reduced productivity at work and increased absenteeism. Outdoor activities may become limited during high pollen seasons, leading to social isolation or a sedentary lifestyle for those who enjoy nature.
Questions to Ask Your Healthcare Provider
To better manage the condition, patients should engage in open dialogue with their healthcare team. Useful questions include:
- What specific allergens are triggering my symptoms, and how can I avoid them?
- How can I tell the difference between my allergies and a sinus infection?
- Are there any side effects I should watch for with my current medications?
- Would I be a good candidate for allergy shots or sublingual immunotherapy?
- How can I safely use over-the-counter decongestants without worsening my symptoms?
Common Questions and Answers
Q: Can you outgrow allergic rhinitis?
A: It is possible for allergy symptoms to diminish or disappear completely as you age, although they can also persist for life or return after a period of remission.
Q: Is allergic rhinitis the same thing as a cold?
A: No, allergic rhinitis is caused by an immune reaction to allergens and does not cause a fever or body aches, whereas a cold is a viral infection that typically resolves within a week.
Q: Can allergies cause a fever?
A: Allergic rhinitis itself does not cause a fever; if a fever is present, it usually indicates a secondary infection such as sinusitis or a viral illness.
Q: Do allergy shots really work?
A: Yes, immunotherapy (allergy shots) is highly effective for many people and is currently the only treatment that changes the immune system's response to allergens, potentially providing long-term relief.
Q: Can moving to a different location cure my allergies?
A: Moving may provide temporary relief if you escape specific local pollens, but individuals prone to allergies often develop new sensitivities to the flora in their new environment within a few years.